Are ILWU members in the healthcare and hotel industry at a greater risk of catching SARS? There are some risks
and ILWU members should know the basic precautions and safety protections to avoid catching SARS (severe acute respiratory syndrome).
As of April 23, 2003, the Hawaii Department of Health reported there are no confirmed cases of SARS in Hawaii. However, five suspect cases, that meet case definition, have been reported to the Centers for Disease Control and
Prevention. All individuals have fully recovered or are expected to do so. The State Department of Health has
increased surveillance efforts and is maintaining daily contact with medical facilities to monitor the situation.
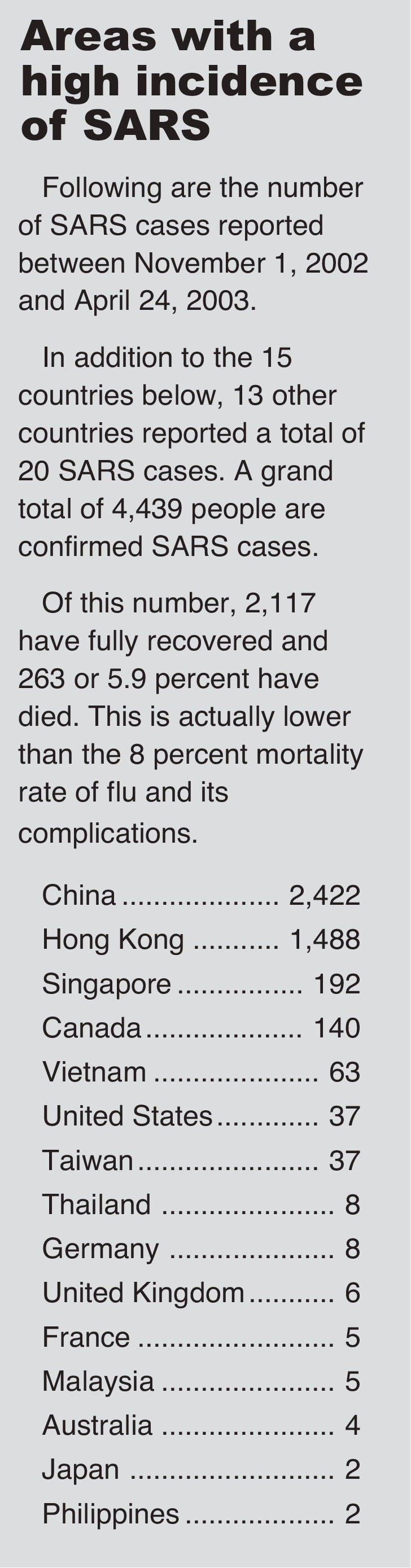
SARS has been getting a lot of attention in the media, and is very serious because of how easily it spreads
and the severity of its symptoms. However, the common flu or influenza is actually more deadly and kills more people than SARS. About 8 percent of the people who get sick with the flu die from the flu or its complications, like
pneumonia. The CDC estimates about 36,000 Americans will die as the result of flu this year. In comparison, a little less than 6 percent of people with SARS have died.
Fortunately, some of the same precautions to avoid SARS should also reduce the number of people who catch
the flu.
Infection control for suspected SARS contacts
Patients with SARS pose a risk of transmission to close household contacts and health care personnel in close
contact. The duration of time before or after onset of symptoms during which a patient with SARS can transmit
the disease to others is unknown. The following infection control measures are recommended for patients with
suspected SARS in households or residential settings.These recommendations are based on the experience in the United States to date and may be revised as more information becomes available.
SARS patients should limit interactions outside the home and should not go to work, school, out-of-home child care, or other public areas until 10 days after the resolution of fever, provided respiratory symptoms are absent or improving. During this time, infection control precautions should be used, as describe below, to minimize the potential for transmission.
All members of a household with a SARS patient should carefully follow recommendations for hand hygiene (e.g., frequent
hand washing or use of alcohol-based hand rubs), particularly after contact with body fluids (e.g., respiratory secretions,
urine, or feces). See the “Guideline for Hand Hygiene in Health-Care Settings” for more details on hand hygiene.
Use of disposable gloves should be considered for any direct contact with body fluids of a SARS patient. However, gloves
are not intended to replace proper hand hygiene. Immediately after activities involving contact with body fluids, gloves should be removed and discarded and hands should be cleaned. Gloves must never be washed or reused.
Each patient with SARS should be advised to cover his or her mouth and nose with a facial tissue when coughing or sneezing.
If possible, a SARS patient should wear a surgical mask during close contact with uninfected persons to prevent spread of infectious droplets. When a SARS patient is unable to wear a surgical mask, household members should wear surgical masks when in close contact with the patient.
Sharing of eating utensils, towels, and bedding between SARS patients and others should be avoided, although such items
can be used by others after routine cleaning (e.g., washing with soap and hot water). Environmental surfaces soiled by body
fluids should be cleaned with a household disinfectant according to manufacturer’s instructions; gloves should be worn during this activity.
Household waste soiled with body fluids of SARS patients, including facial tissues and surgical masks, may be discarded
as normal waste.
Household members and other close contacts of SARS patients should be actively monitored by the local health department for illness.
Household members or other close contacts of SARS patients should be vigilant for the development of fever or respiratory
symptoms and, if these develop, should seek healthcare evaluation. In advance of evaluation, healthcare providers should be
informed that the individual is a close contact of a SARS patient. Household members or other close contacts with symptoms of SARS should follow the same precautions recommended for SARS patients.
At this time, in the absence of fever or respiratory symptoms, household members or other close contacts of SARS patients need not limit their activities outside the home.